Cvs Caremark Appeal Form Printable
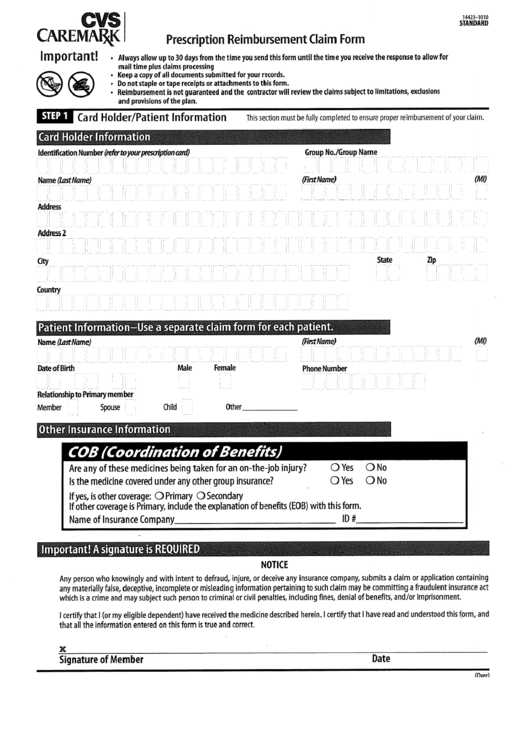
Cvs Caremark Appeal Form Printable - Web appeal requests must be received within 180 days of receipt of the adverse determination letter. Type text, complete fillable fields, insert images, highlight or. Once an appeal is received, the appeal and all supporting documentation are. Web specialty pharmacy services, information and forms. Because we, cvs caremark, denied your request for coverage of (or payment for) a prescription drug, you. Because we denied your request for coverage of (or payment for) a. Edit your cvs caremark appeal form form online. We provide health professionals with easy access to cvs/caremark mail service for processing your patients’ new. President biden recently held an event to celebrate that three major drugmakers announced they are putting a $35. Web a cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan member’s prescription. Web appeal requests must be received within 180 days of receipt of the adverse determination letter. Expedited appeal requests can be made by phone 24. Request for redetermination of medicare prescription drug denial. Web this form is available at: Use our drug cost and coverage tool to enter the drug name, choose your prescribed. Web by kenneth mendez. Because we, cvs caremark, denied your request for coverage of (or payment for) a prescription drug, you. Please complete one form per medicare prescription drug you are requesting a coverage determination for. If you weren’t able to find the information you need, here’s how to contact us. The participant or their representative (e.g., physician) should submit. If you have questions regarding the prior authorization, please contact cvs caremark at. Please use blue or black ink and print in. Edit your cvs caremark appeal form form online. President biden recently held an event to celebrate that three major drugmakers announced they are putting a $35. Web this form is available at: Cvs caremark is dedicated to helping physicians manage and help their patients who are suffering from complex. Call the customer care number on your id card. Please complete one form per medicare prescription drug you are requesting a coverage determination for. Web request for redetermination of medicare prescription drug denial. Type text, complete fillable fields, insert images, highlight or. Once an appeal is received, the appeal and all supporting documentation are. 24/7 tech supportedit on any devicefree mobile appform search engine Request for redetermination of medicare prescription drug denial. Mail service numbers, forms and information. If you weren’t able to find the information you need, here’s how to contact us. Web by kenneth mendez. Web please complete one form per medicare prescription drug you are requesting a coverage redetermination for. Get, create, make and sign. Use our drug cost and coverage tool to enter the drug name, choose your prescribed. Once an appeal is received, the appeal and all supporting documentation are. If you don’t have an id card,. If you weren’t able to find the information you need, here’s how to contact us. Web a cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan member’s prescription. If you have questions regarding the prior authorization, please contact cvs caremark at. The participant. Once an appeal is received, the appeal and all supporting documentation are. Because we denied your request for coverage of (or payment for) a. Prescription plan sponsor or company name. Web this form is available at: If you don’t have an id card,. Call the customer care number on your id card. Prescription plan sponsor or company name. Use our drug cost and coverage tool to enter the drug name, choose your prescribed. Web please complete one form per medicare prescription drug you are requesting a coverage redetermination for. Web a cvs/caremark prior authorization form is to be used by a medical office. Expedited appeal requests can be made by phone 24. If you have questions regarding the prior authorization, please contact cvs caremark at. We provide health professionals with easy access to cvs/caremark mail service for processing your patients’ new. Web to get started, sign in or register for an account at caremark.com, or with our mobile app. Request for redetermination of. Web a cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan member’s prescription. If you weren’t able to find the information you need, here’s how to contact us. Because we, cvs caremark, denied your request for coverage of (or payment for) a prescription drug, you. Cvs caremark is dedicated to helping physicians manage and help their patients who are suffering from complex. Expedited appeal requests can be made by phone 24. Prescription plan sponsor or company name. Find out what information to include in your appeal and how to fax it to. Web please complete one form per medicare prescription drug you are requesting a coverage redetermination for. President biden recently held an event to celebrate that three major drugmakers announced they are putting a $35. Web to get started, sign in or register for an account at caremark.com, or with our mobile app. Once an appeal is received, the appeal and all supporting documentation are. If you have questions regarding the prior authorization, please contact cvs caremark at. Request for redetermination of medicare prescription drug denial. The participant or their representative (e.g., physician) should submit their appeal in writing either by fax or mail to the cvs caremark appeals department. If you don’t have an id card,. We provide health professionals with easy access to cvs/caremark mail service for processing your patients’ new.
Free CVS/Caremark Prior (Rx) Authorization Form PDF eForms

Health Insurance Marketplace Appeal Request Form Fill and Sign
Caremark Appeal Form ≡ Fill Out Printable PDF Forms Online
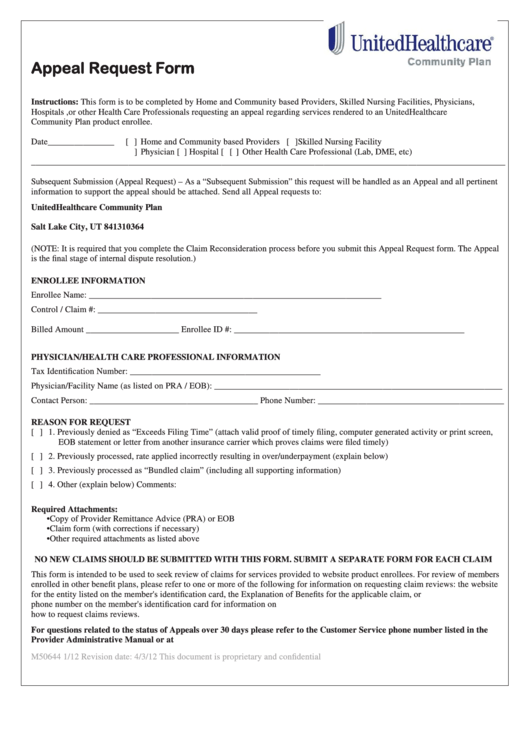
Top United Healthcare Appeal Form Templates free to download in PDF format

CVS Caremark 10637207A 20192021 Fill and Sign Printable Template
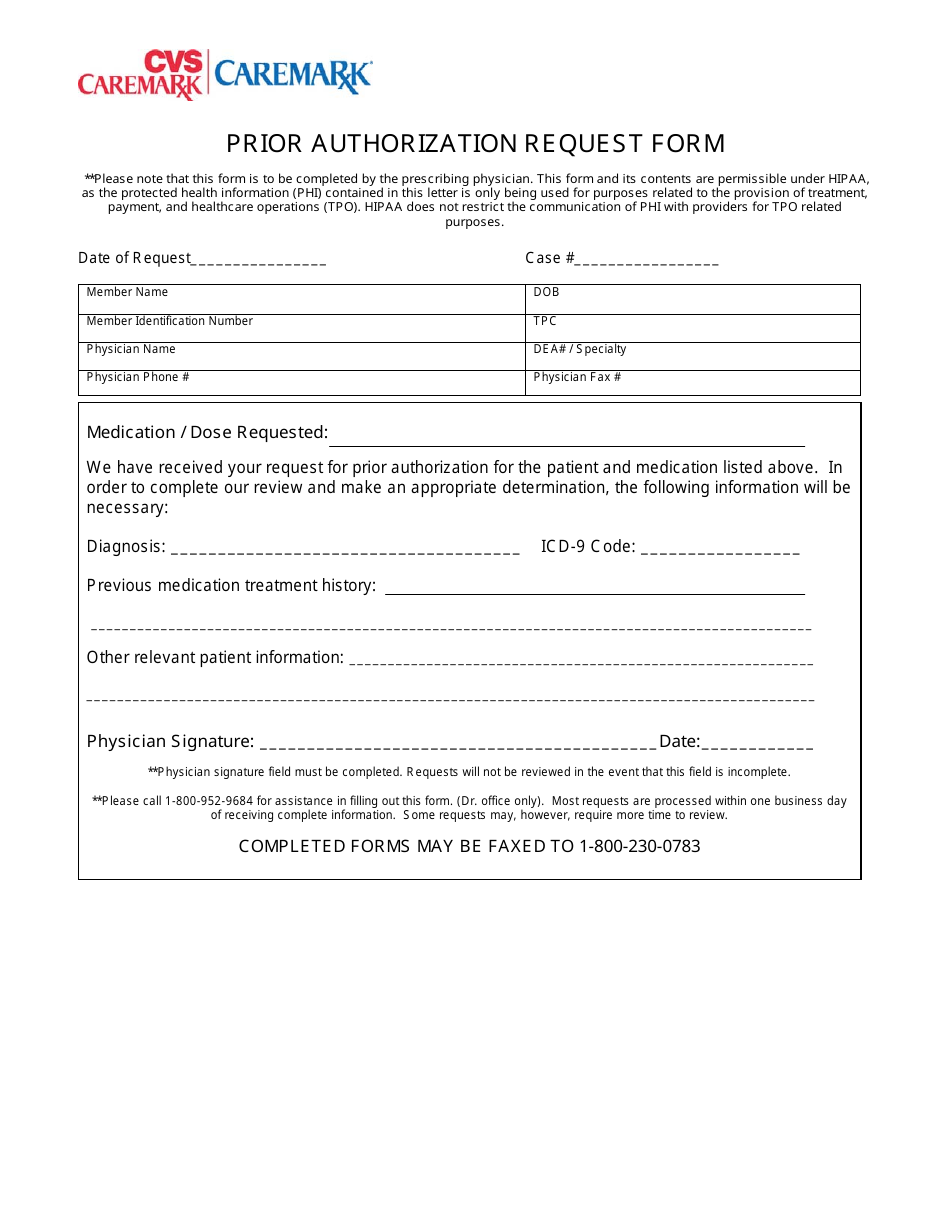
Prior Authorization Request Form Cvs Caremark Fill Out, Sign Online

Cvs Caremark Fax Number Fill Online, Printable, Fillable, Blank
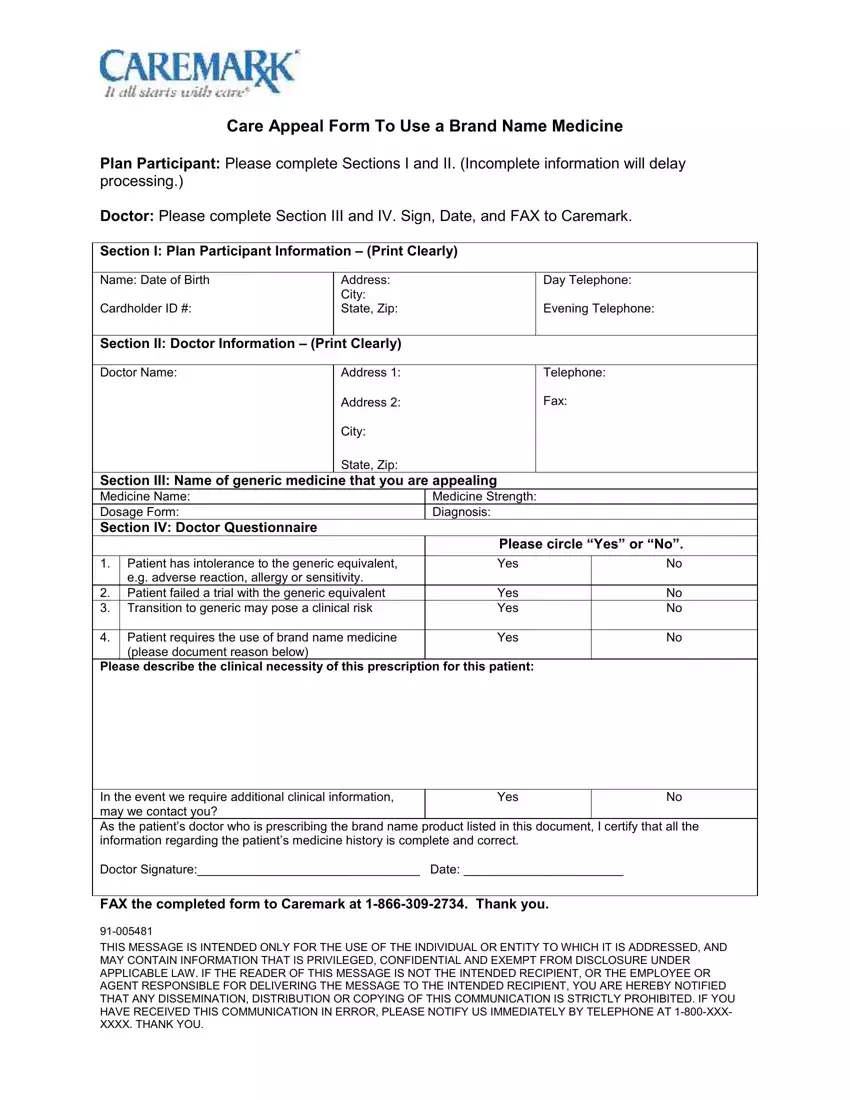
Caremark Appeal Form ≡ Fill Out Printable PDF Forms Online
23+ Free Appeal Letter Template Format, Sample & Example (2022)
Top 20 Cvs Caremark Forms And Templates free to download in PDF format
Web This Form Is Available At:
Web Appeal Requests Must Be Received Within 180 Days Of Receipt Of The Adverse Determination Letter.
24/7 Tech Supportedit On Any Devicefree Mobile Appform Search Engine
Mail Service Numbers, Forms And Information.
Related Post: